Shoulder Rehab Exercises After Dislocation: Your Complete Recovery Guide
Recovering from a shoulder dislocation requires a structured, progressive approach to restore stability, strength, and function. Shoulder rehab exercises after dislocation play a crucial role in preventing re-injury and ensuring a successful return to daily activities and sports. This comprehensive guide outlines evidence-based rehabilitation strategies, specific exercises for each recovery phase, and essential safety considerations to help you navigate your shoulder recovery journey effectively.
Shoulder dislocations are among the most common joint injuries, affecting athletes and non-athletes alike. Whether you've experienced an anterior, posterior, or inferior dislocation, proper rehabilitation is essential for optimal healing and long-term joint stability. Research shows that structured exercise programs significantly reduce recurrence rates and improve functional outcomes compared to passive recovery approaches.
Read Also || Mastering Thoracic Spine Mobility for a Stronger, Safer Overhead Press
Understanding Shoulder Dislocation and Recovery Process
A shoulder dislocation occurs when the head of the humerus (upper arm bone) is forced out of the shallow socket of the shoulder blade. This injury typically damages surrounding soft tissues, including ligaments, joint capsule, and sometimes the rotator cuff muscles. The recovery process involves tissue healing, inflammation reduction, and gradual restoration of mobility and strength.
The healing timeline varies based on several factors, including age, severity of injury, associated tissue damage, and adherence to rehabilitation protocols. Recovery typically spans 12-16 weeks for most patients, though complete functional restoration may take up to six months. Understanding this timeline helps set realistic expectations and promotes consistent participation in rehabilitation exercises.
Types and Severity Impact Recovery
Anterior dislocations account for approximately 95% of shoulder dislocations and typically require 3-4 weeks of initial immobilization. Posterior dislocations are less common but may require longer protection periods due to associated bone or soft tissue damage. The presence of additional injuries, such as Hill-Sachs lesions or Bankart tears, may extend recovery time and influence exercise selection.
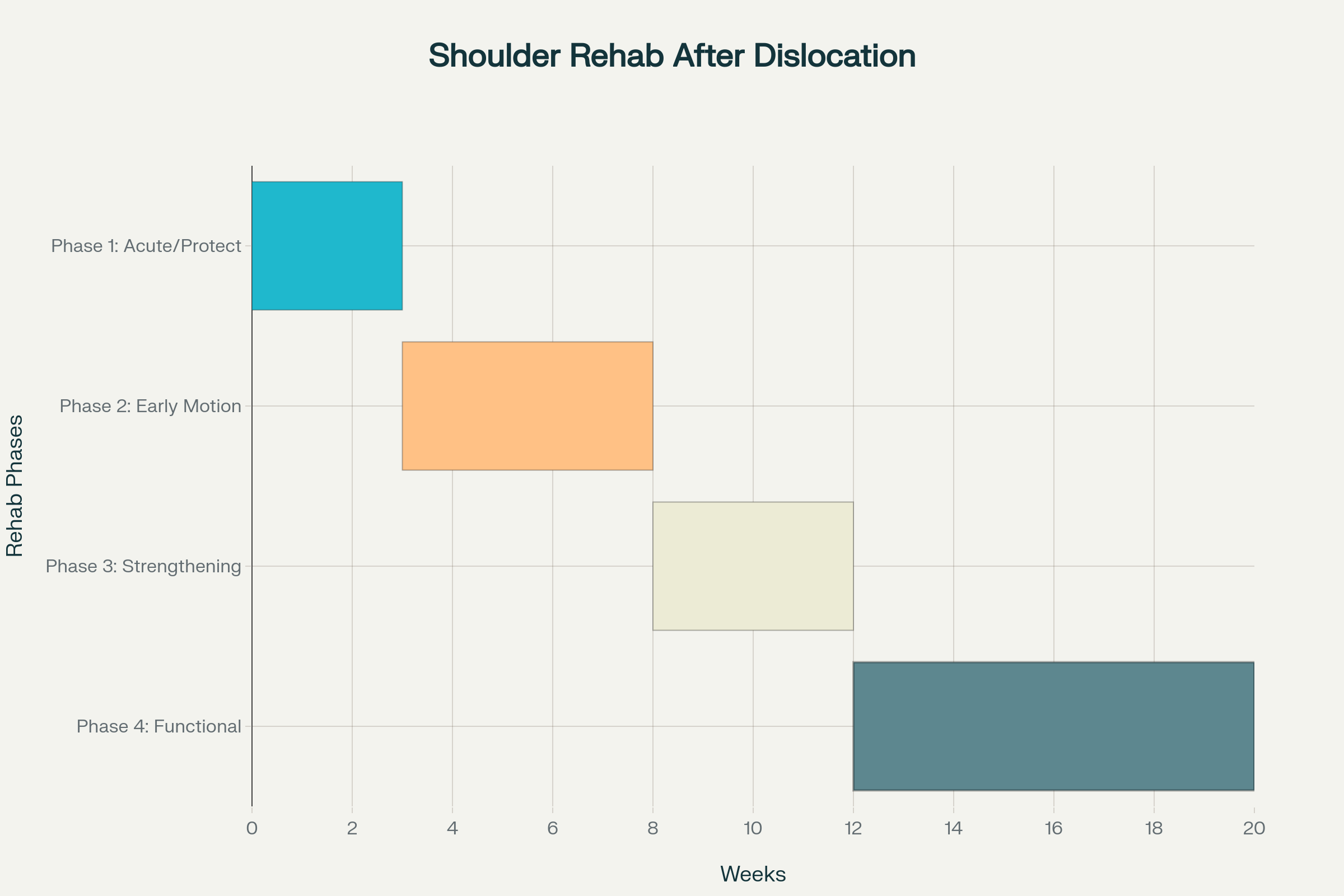
The Four-Phase Rehabilitation Approach
Successful shoulder rehabilitation after dislocation follows a systematic, phase-based approach that progressively challenges the healing tissues while maintaining safety. Each phase has specific goals, timeframes, and exercise protocols designed to optimize recovery outcomes.
Phase 1: Acute Protection Phase (0-3 Weeks)
During the acute phase, primary goals include pain management, inflammation control, and tissue protection. Most patients wear a sling for immobilization, though the duration varies based on age and injury severity. Younger patients typically require 3-4 weeks of immobilization, while those over 40 may only need 1-2 weeks to prevent secondary stiffness.
Safe exercises during this phase include:
Pendulum exercises: Allow gravity to gently move the arm without active muscle contraction
Gentle finger and wrist movements: Maintain circulation and prevent stiffness
Isometric contractions: Light muscle activation without joint movement
Elbow range of motion: Bend and straighten the elbow to prevent stiffness
Pain serves as the primary guide during this phase. Any exercise that increases pain or reproduces the dislocation mechanism should be avoided. Ice application for 15-20 minutes after exercise sessions helps control inflammation and provides pain relief.
Phase 2: Early Motion Phase (3-8 Weeks)
As pain subsides and initial healing occurs, the focus shifts to restoring passive range of motion and beginning gentle strengthening. This phase requires careful progression to avoid re-injury while preventing long-term stiffness and weakness.
Key exercises include:
Wall slides: Facing a wall, slide your arm up while maintaining contact with the surface
Scapular setting: Squeeze shoulder blades together to activate stabilizing muscles
Passive external rotation: Use the uninjured arm to gently move the affected shoulder
Towel stretches: Gentle cross-body stretches to improve flexibility
Range of motion goals for this phase include achieving 90 degrees of forward flexion and 30-45 degrees of external rotation. Progression should be gradual and pain-free, with most patients reaching these milestones by 6-8 weeks post-injury.
Phase 3: Strengthening Phase (8-12 Weeks)
The strengthening phase emphasizes building muscle strength, endurance, and neuromuscular control. Rotator cuff strengthening exercises become the primary focus, as these muscles provide critical dynamic stability to the shoulder joint.
Progressive strengthening exercises include:
Resistance band external rotation: Start with light resistance and progress gradually
Internal rotation exercises: Strengthen the subscapularis muscle
Scapular strengthening: Target middle trapezius, rhomboids, and serratus anterior
Prone T, Y, and I exercises: Strengthen posterior shoulder and upper back muscles
Research demonstrates that resistance band exercises are particularly effective for rotator cuff strengthening, providing variable resistance that matches muscle strength curves. Begin with the lightest resistance band and progress to heavier bands as strength improves.
Phase 4: Functional Phase (12+ Weeks)
The final phase prepares patients for return to full activities, including sports participation. Sport-specific rehabilitation exercises become increasingly important during this phase, with emphasis on movement patterns and demands specific to individual activities.
Advanced exercises include:
Plyometric training: Explosive movements to prepare for high-level activities
Proprioceptive challenges: Balance and coordination exercises
Multi-directional strengthening: Complex movement patterns
Graduated return to activity protocols: Systematic progression back to full participation
Exercise Technique and Safety Guidelines
Proper exercise technique is crucial for safety and effectiveness throughout all rehabilitation phases. Common mistakes that delay recovery include progressing too quickly, using excessive force, and returning to high-risk activities prematurely.
Essential Safety Principles
Always warm up before exercises using gentle range of motion movements or heat application for 5-10 minutes. This increases blood flow and tissue pliability, reducing injury risk during exercise.
Respect pain limits throughout the rehabilitation process. Mild discomfort is normal, but sharp pain or reproduction of dislocation symptoms indicates excessive stress on healing tissues. Stop immediately and consult your healthcare provider if concerning symptoms occur.
Avoid risky positions during early rehabilitation phases. The combination of shoulder abduction (arm out to the side) and external rotation (rotation away from the body) recreates the position of injury and should be avoided until adequate healing has occurred.
Progress gradually through each phase, meeting specific criteria before advancement. Rushing through rehabilitation phases significantly increases re-injury risk and may result in chronic instability.
Professional Guidance and Monitoring
While many exercises can be performed independently, professional supervision is highly recommended for optimal outcomes. Physical therapists specializing in shoulder rehabilitation can provide manual therapy techniques, advanced exercise progressions, and objective assessments of recovery progress.
When to Seek Professional Help
Immediate medical attention is warranted if you experience severe pain, numbness, tingling, or weakness in the arm or hand. These symptoms may indicate nerve damage or vascular compromise requiring urgent evaluation.
Other indications for professional consultation include:
Lack of improvement after 2-3 weeks of consistent exercise
Recurrent episodes of shoulder instability
Inability to achieve expected range of motion milestones
Persistent pain that limits daily activities
Return to Sport Considerations
Athletes face unique challenges when returning to sport after shoulder dislocation. Return to play decisions should be based on objective criteria rather than time alone, including full pain-free range of motion, symmetric strength compared to the uninjured side, and successful completion of sport-specific functional tests.
Research indicates that premature return to sport significantly increases re-injury rates, with some studies reporting recurrence rates as high as 90% in young athletes who return too early. Most experts recommend a minimum of 3-4 months before return to contact sports, with longer periods for overhead sports like baseball or swimming.
Long-Term Prevention Strategies
Preventing future shoulder dislocations requires ongoing attention to strength, flexibility, and movement quality. Maintenance exercise programs should continue indefinitely, with particular focus on rotator cuff and scapular stabilizer strength.
Key prevention strategies include:
Regular performance of shoulder strengthening exercises
Proper warm-up before athletic activities
Technique modification in high-risk sports
Use of protective equipment when appropriate
Recognition and avoidance of positions that increase re-injury risk
Frequently Asked Questions
1. How long does it take to recover from a shoulder dislocation?
Recovery time varies but typically requires 12-16 weeks for most people to return to full activities. Complete healing and strength restoration may take up to 6 months. Factors affecting recovery include age, severity of injury, associated damage, and adherence to rehabilitation protocols.
2. Can I do shoulder rehab exercises at home without supervision?
Basic exercises can be performed at home, but professional guidance is recommended, especially during early phases. A physical therapist can ensure proper technique, provide manual therapy, and modify exercises based on your specific needs and progress.
3. What exercises should I avoid after a shoulder dislocation?
Avoid the apprehension position (arm out to the side with external rotation), overhead reaching, and any movements that reproduce dislocation symptoms. High-impact activities, contact sports, and heavy lifting should be avoided until cleared by your healthcare provider.
4. How do I know if I'm progressing my exercises too quickly?
Warning signs include increased pain lasting more than 2 hours after exercise, swelling, warmth in the joint, or feelings of instability. Pain should gradually decrease over time, and you should notice improvements in range of motion and strength with consistent exercise.
5. Are resistance bands better than weights for shoulder rehabilitation?
Resistance bands are often preferred during early rehabilitation because they provide variable resistance and are gentler on healing tissues. They're also convenient and allow for sport-specific movement patterns. Weights can be incorporated in later phases for more advanced strengthening.
6. When can I return to sports after a shoulder dislocation?
Return to sport timing depends on the specific sport and your individual progress. Non-contact sports may be resumed after 2-3 months, while contact sports typically require 4-6 months. Return should be based on achieving specific criteria rather than time alone.
7. What's the difference between a subluxation and a dislocation?
A dislocation involves complete separation of the joint surfaces, while a subluxation is a partial dislocation where the joint surfaces temporarily separate but spontaneously relocate. Both require rehabilitation, though subluxations may have shorter recovery periods.
8. How often should I do my rehabilitation exercises?
Exercise frequency depends on the rehabilitation phase. Early phases may require 2-3 short sessions daily, while later phases might involve 1 comprehensive session per day. Your healthcare provider will prescribe the appropriate frequency based on your specific needs.
9. Can a dislocated shoulder heal without surgery?
Many shoulder dislocations heal successfully with non-surgical treatment, especially first-time dislocations in older patients. However, young athletes or those with recurrent dislocations may benefit from surgical stabilization to reduce re-injury risk.
10. What are the long-term complications of shoulder dislocation?
Potential complications include recurrent instability, chronic pain, reduced range of motion, and early onset arthritis. However, proper rehabilitation significantly reduces these risks. Most people achieve excellent long-term outcomes with appropriate treatment and consistent exercise.
Conclusion
Shoulder rehab exercises after dislocation are essential for restoring function, preventing re-injury, and ensuring long-term shoulder health. Success depends on following a structured, progressive rehabilitation program that respects tissue healing while systematically challenging the recovering shoulder. Remember that recovery is a process requiring patience, consistency, and often professional guidance.
The key to successful recovery lies in understanding that each phase serves a specific purpose in the healing process. Attempting to rush through phases or skip steps significantly increases the risk of re-injury and chronic problems. By following evidence-based rehabilitation protocols and maintaining realistic expectations, most people can achieve excellent outcomes and return to their desired level of activity.
Whether you're an athlete looking to return to competition or someone seeking to regain normal daily function, the investment in proper rehabilitation pays dividends in long-term shoulder health and quality of life.




Comments
Post a Comment